At Federal Medical Center Devens, a federal prison in Massachusetts, there is a prisoner who thinks he is a warden. “I’m the boss. I’m going to fire you,” Victor Orena, who is 89, will tell the prison staff.
On some days, Mr. Orena is studiously aloof — as if he were simply too busy or important to deal with anybody else. On other days, he orders everyone around in an overwrought Mafioso tone: a version of the voice that, perhaps, he used when he was a working New York City mob boss decades ago, browbeating members of his notorious crime family. This makes the real prison warden laugh.
On a recent morning, Mr. Orena sat in his wheelchair beside a man with bloodshot eyes. I asked them if they knew where they were.
“This is a prison,” Mr. Orena said, brightly.
“Why are you here?” I asked.
“I don’t remember,” he frowned. “I don’t know.”
Timothy Doherty, a senior officer specialist at F.M.C. Devens, which houses federal prisoners who require medical care, estimates that 90 percent of the men he oversees “don’t know what they did. Some of them don’t even know where they are.” Mr. Doherty helps to run the Memory Disorder Unit, the federal prison system’s first purpose-built facility for incarcerated people with Alzheimer’s disease and other forms of dementia.
Down the hall from where Mr. Orena was sitting — past the activity room with the fish tank, where a cluster of men were watching “King Kong” on TV — there is a cell belonging to another man who wakes every day to discover anew that he is in prison. Some mornings, the man packs up his belongings and waits at the door. He explains that his mother is coming to get him.
“She sure is,” a staff member might say, before slowly leading him back to his cell.
In recent years, I have reported on many aspects of life with dementia. One image has especially haunted me: that of a prisoner who, as a result of cognitive impairment, no longer remembers his crimes — but is still being punished for them.
We don’t know exactly how many people in American prisons have dementia because nobody is counting. By some estimates, there are already thousands, most of them languishing in the general inmate population.
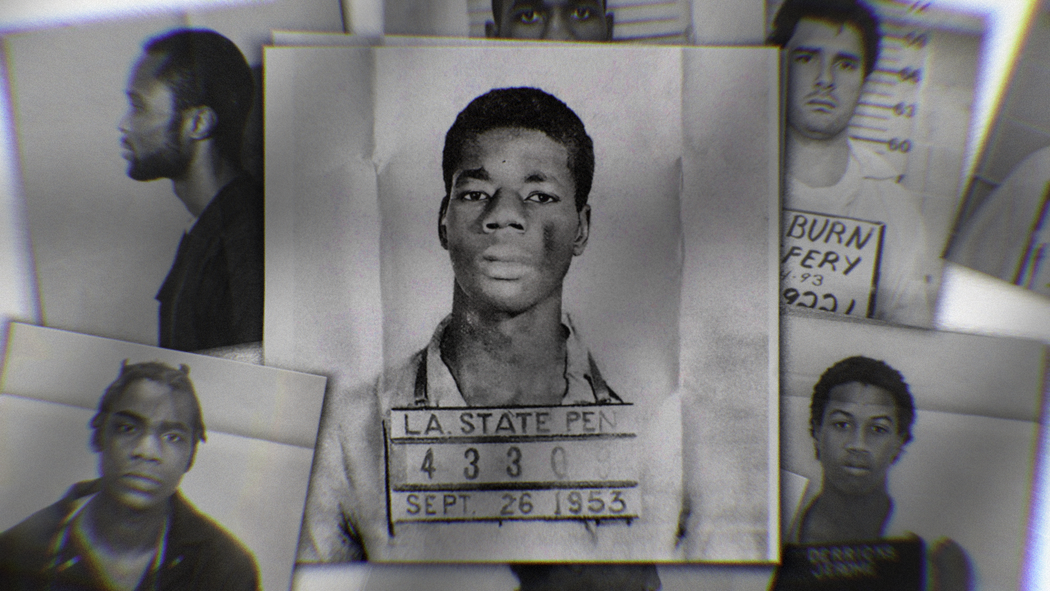
Older adults represent one of the fastest-growing demographic groups within American correctional facilities. Between 1999 and 2016, the number of prisoners over 55 increased by 280 percent, according to a report by the Pew Charitable Trusts; over the same period, the number of incarcerated younger people grew by just 3 percent. This trend is largely attributed to “tough on crime” reforms in the 1980s and 1990s, which lengthened sentences and ensured that many more people would grow old and frail and then die behind prison walls.
Incarcerated life is also thought to accelerate the aging process, such that many longtime prisoners appear more than a decade older than their chronological ages — and are considered “elderly” at 50 or 55.
Early on, a prisoner’s dementia might go unnoticed. Federal prisons do not routinely screen older people for Alzheimer’s disease and other forms of dementia unless they exhibit symptoms. And the rigidity and monotony of institutional life can often mask them: A person can get by, for a while, just by following the man ahead of him.
But later, things will start to fall apart. At first, a person with dementia might struggle in the normal way that other aging prisoners do: to walk long distances for meals or medication, to get up from a low-lying toilet without a handrail, to climb a bunk bed on command. Over time, he might start to pace or repeat phrases over and over. He might have hallucinations or delusions or paranoia. He might fall. He might be incorrectly medicated by a doctor who does not understand his condition. He might struggle to distinguish between items of similar color — mashed potatoes on a white plate, say — and so have trouble eating. Or forget to eat at all.
A prisoner with dementia might wear slippers outside his cell, even though this is against the rules. Or wander somewhere he is not supposed to go. He might have trouble judging the distance between things and bump into people who might, in turn, mistake the stumbles for deliberate affronts. He might begin to smell, because he can’t remember how to wash his body — and he might expose his body to others, because his disease leaves him sexually disinhibited. He might get hurt by another prisoner who takes advantage of his impairment and then forget that he was hurt. He might hurt someone else. He might become incontinent. He might grow afraid of shadows because he perceives them to be holes in the ground.
Eventually, the man will find himself living inside an unyielding system whose boundaries and principles he can no longer see or interpret or remember. And because he can’t stop breaking the rules, he might be punished — in some cases, with solitary housing. There, his condition might worsen. “Noncompliance with correctional rules and directions is often treated as a disciplinary issue rather than a medical issue,” explains a 2022 report, “Persons Living With Dementia in the Criminal Legal System,” copublished by the American Bar Association Commission on Law and Aging. Because the prisoner has nowhere else to go, he might muddle along as best as he can until he becomes so impaired that he is transferred to a medical center, where he will spend the rest of his incarcerated days lying in bed.
The Memory Disorder Unit at F.M.C. Devens, which opened in 2019 and was designed to resemble a memory care facility, offers an alternative path for such a prisoner. Its correctional officers have received training from the National Council of Certified Dementia Practitioners and currently supervise around two dozen men with an average age of 72. These officers have been given a tall task: to bend an institution designed to punish and sequester into a place that can provide care to some of the most vulnerable people in the system.
In the end, they are proud of what they have built. Why else would they let a journalist come to see it? And still, the M.D.U. seems to challenge several of the classic justifications for the prison system itself: to segregate the dangerous, for instance (many M.D.U. residents are weak and unthreatening), or to reform the morally corrupt (many M.D.U. prisoners don’t remember doing wrong).
Amy Boncher, who was the warden of F.M.C. Devens when I visited in May (she is now the Bureau of Prisons’ Northeast regional director), told me that when she first met the residents of the unit, it was hard to make sense of the entire project. “I looked at them. And I’m thinking: Why haven’t we released all of them?”
“Do you know history?” An M.D.U. resident shuffled toward me. I could only make out bits of speech: “Fidel Castro” and “revolution” and “United States took over Cuba.” This man was born in Cuba and now spends his days reliving its past. As he moved closer, I noticed the smell; since arriving at the M.D.U., he has generally refused to brush his teeth.
I’m told that he’s a “big teddy bear” — though he can get agitated if, say, another prisoner gets annoyed by his revolutionary babble and tells him that Fidel Castro is dead and that nobody liked him. When this happens, a staff member will play the man some old Cuban music, and he will weep as he listens to it.
Most days, he doesn’t seem to know why he is in prison, though sometimes he will allude to a past transgression. “I was a young man,” he will insist. “I told them who did it.”
After a few minutes, an “inmate companion” named Oswaldo Ornelas put his arm around the Cuban man’s shoulders and led him down the hallway. Mr. Ornelas is one of four cognitively healthy prisoners, men without dementia, who are trained to live and work in the M.D.U. in exchange for $30 to $100 a month in wages and, possibly, time off their sentences. The companions are selected based on criminal history — they can’t have been convicted of a sex crime or another violent crime — and temperament. “You’ve got to make sure they won’t take advantage of the men in any way,” Mr. Doherty, the senior officer specialist, said.
Mr. Ornelas told me that a few years ago, while incarcerated, he received a kidney transplant and that he wanted to work in the M.D.U. “to give my life back.”
When I arrived at the unit, Mr. Ornelas was on duty with another companion, Richard Lotito, and the two men had just spent three hours waking, showering and dressing the other prisoners. Their work is physically demanding and exquisitely intimate. Several of the men need help with the toilet and wear diapers. Over many months, the companions have learned their individual needs and tempos. “One guy poops every other day, another poops all day,” Mr. Lotito said. Another gets confused and urinates in the trash cans. “The key to this job is patience.” (Mr. Lotito and Mr. Ornelas were both released in July.)
The M.D.U. is made up of two long hallways that are lined with cells and several common rooms. Unlike standard prison units, the M.D.U. has a kitchen filled with snacks, because sometimes the men forget that they have just eaten and insist that they are starving — and then one of the companions can make them peanut butter sandwiches.
Across most of the unit, the walls are painted a pale pink. In the world of dementia care, pink is sometimes thought to be a calming color that reduces combative behavior. Two officers and one nurse are walking the floors at any given moment, but they do not carry guns, and they are not everywhere. Near the entryway, the prisoners’ artwork is displayed on the wall: paper lanterns, painted tiles, flowers made of pipe cleaners. On the doors to the cells are pictures of favorite objects that help the men to locate their rooms: a Cadillac, the Red Sox logo, an umbrella. Most of the time, the doors inside the unit are unlocked, and the prisoners can come and go as they please. If the whole place weren’t locked down and made of windowless concrete, it would almost look like a day care center.
During the day, there are activities. Trivia, with questions about events from the ’50s and ’60s. Bocce ball. Music therapy. Outside of scheduled time, the men are encouraged to be active. One folds laundry. One sits on the patio on a metal rocking chair and watches birds fly by. Another is given a paintbrush and a can of washable paint so that he can paint the walls all day — “because he gets upset when he’s bored and doesn’t know what to do with himself,” Mr. Doherty said.
As I was led around the unit, I heard screaming. I was told that the screaming man had suffered a brain injury and that he screams often, sometimes because of pain from the spots on his legs where he has rubbed the skin raw. Alexandra Kimball, an occupational therapist, rushed to his side. “Do you like Tom Brady?” she asked gently, referring to the former N.F.L. quarterback.
The screaming stopped. “I love Tom Brady.”
The staff members of the M.D.U. maintain a binder with profiles of the prisoners, including information on how to soothe them. The binder entry for the screaming man advises officers to reference Tom Brady.
Compared to officers in the rest of the prison, M.D.U. staff members can exercise a bit more discretion when it comes to rule breaking. Ms. Boncher, the former warden, told me that the M.D.U. has its own unique “disciplinary procedures.” Her staff members, she explained, are skilled at deciding which prisoners should be disciplined for bad behavior, which she says involves a psychological determination about whether the offending man knew that he was doing something wrong and did it anyway and is therefore responsible and worthy of punishment or was simply acting on impulse, a victim of his own damaged mind. This approach assumes that it is even possible to deduce the mental state of a man who only sometimes or partially understands himself.
But sometimes the M.D.U. residents will fight in the TV room. Or someone will spit on someone else — or walk into the wrong cell and get punched in the face. In most cases, a man who acts out will be “redirected” to a new activity. In other cases, he will lose his commissary or phone privileges for a few days. In rarer cases, he will be locked alone in his room until he calms down, an approach that would not be used in a typical nursing home.
A few men are only allowed out of their cells for two hours each day, with supervision. This includes someone whom Mr. Doherty describes as “absolutely the nicest of inmates” until he starts hearing voices. Some of the men understand that they are being punished and some don’t, and some understand but then forget.
“All the prisons need this,” Mr. Doherty told me, gesturing around him. “What do other places do with these guys?”
On the day I visited the unit, a few of the medical staff members told me that they previously worked in community nursing homes and that the M.D.U. prisoners are probably receiving better care than they would on the outside, in whatever Medicaid-subsidized beds they were likely to find themselves. Behind bars, the men have easy access to psychologists, social workers and a pharmacist with a specialty in geriatrics. Perhaps that’s true. And yet, the existence of the M.D.U. seems to impugn the basic logic of the carceral system or at least its classic rationales.
For some, the point of prison is chiefly to incapacitate dangerous people. The men inside the M.D.U. vary in their physical abilities, but many are very sick and confused and use wheelchairs or walkers, and they probably couldn’t hurt anyone if they wanted to. With them, appeals to public safety fall short. More broadly, the Department of Justice has concluded that “aging inmates are generally less of a public safety threat.” And researchers have found that recidivism rates drop to nearly zero for people over 65.
For others, prison is meant to offer retribution for wrongdoing. In this view, if a person does something wrong, he deserves to be punished in proportion to his crime — and justice depends on it. Dementia tests this logic in different ways. Proponents of this view might decide that even a just act of punishment becomes unjust if the offender no longer understands why he is being condemned. Alternatively, they might conclude that those who are ailing and weak deserve mercy. Many of the M.D.U. residents have already served several years of their sentences.
Some believe that incarceration is an opportunity for rehabilitation. “But with dementia, there is no rehabilitation,” says Lynn Biot-Gordon, of the National Council of Certified Dementia Practitioners, the organization that provided training to M.D.U. staff. Moral education is impossible for a person who cannot be educated. And a prisoner cannot reflect on his crimes — and then maybe regret them or feel ashamed of them or be repulsed by them or resolve to do better in the future — if he does not even remember them or feel responsible for them.
Kelly Fricker, a psychologist at F.M.C. Devens, told me that she can’t do much in the way of talk therapy for her M.D.U. patients. “An inherent part of mental health therapy would be to remember from session to session. Many guys here don’t even know who I am.”
But what if the point of imprisoning people for decades is to deter others from committing crimes? Arguably, this rationale survives. Letting the M.D.U.’s prisoners go would, in this view, weaken the overall deterrent effect of criminal law. To hold this view, however, you would have to hold the unlikely belief that a person’s decision to commit a crime would be affected by the knowledge that prisoners with advanced dementia are sometimes released from prison early.
Of course, dementia is not the only medical condition that casts doubt on the principles of incarceration. A prisoner who is very old but cognitively healthy might be similarly frail and unthreatening — or might have changed in drastic ways since his incarceration. A person with a severe mental illness might similarly forget his crimes — or feel psychically disconnected from them or be incapable of thoughtfully reflecting on them later. But dementia might pose the paradigmatic challenge.
Within the philosophical literature on cognitive impairment, there is a debate about whether a person with advanced dementia is even the same person as he was before it. If he cannot be considered the same person, then the men of the M.D.U. are, in an important sense, being punished for someone else’s crimes.
At one point during my visit, I spoke with a white-haired man who had a large nose and reddish skin. “I want to go home like anything,” he told me softly.
“What brought you here?” I asked.
“What brought me here?” The man paused. “Hmm. I don’t know.”
As we walked away, Mr. Doherty shook his head. “He remembers,” he said. Then he told me that the white-haired man had raped his granddaughter.
Later, I wondered how much it should matter whether the old man remembered what he did. And what if he remembered sometimes but not other times? Many people with dementia exist in a kind of middle ground of partial comprehension or have memories that surface and then disappear.
“We get into difficult metaphysical questions about personhood here,” said Jeffrey Howard, a professor of political philosophy and public policy at University College London, when I told him about my conversation with the white-haired man. “But you might think that there are two versions of the man: One of them deserves the punishment, and the other doesn’t. In order to punish the version of him that deserves it, you have to take along this hostage for the ride. It’s hard to see how that sort of collateral damage could be justified.”
There is, technically, a way out. A few of the M.D.U.’s residents have received so-called compassionate release, which allows prisoners with extraordinary or compelling reasons, such as severe illness, to be released early from their sentences. The Federal Bureau of Prisons and most state systems have a version of it. But compassionate release, according to the 2022 American Bar Association report, is “rarely used,” and many prisoners die over the months it takes for their applications to be reviewed. Release is especially rare for people with dementia, because the Bureau of Prisons has historically misinterpreted the federal statute to mean that only prisoners who are terminally ill and very close to death are eligible.
State programs are also limited. Lilli Paratore, the director of legal services at UnCommon Law, which offers pro bono legal representation to incarcerated people in California, told me about representing a woman with Parkinson’s disease and dementia who applied for medical parole. Parole board members looked at her client’s memory gaps with suspicion, Ms. Paratore told me. “Your lack of memory appears to be selective,” one commissioner said. (The client was eventually released.)
Even people with dementia who do obtain early release can find themselves stuck in prison, because they can’t be released without a plan and there is nowhere else for them to go. Some have lost contact with family members. They don’t have anyone on the outside who is able to provide or fund round-the-clock care. And nursing homes usually won’t take them, particularly if they have violent histories — which some but not all of the M.D.U. residents do. “Some people get released but we can’t find them a spot,” Christina Cozza, a social worker in the unit, said.
Within the medical field, there has been very little research on how a history of violence might present itself in the context of dementia. Would a violent impulse be heightened or diminished as the brain it dwells in grows more impaired?
Patricia Ruze, the clinical director of F.M.C. Devens, does not believe that the men of the M.D.U. pose a threat to anyone. “They are probably better behaved than most patients in dementia units generally, because a lot of them have spent many, many, many years in custody and so are rule followers.” Dr. Ruze thinks it would be “totally appropriate” to release the whole unit on compassionate grounds and relocate the men to community nursing homes, which already have experience dealing with aggressive behaviors brought on by cognitive impairment — and which cost much less than operating a prison unit.
“It doesn’t make sense for our country to pay so much to house 15, 20 guys,” Dr. Ruze said.
Ms. Boncher, the former warden, is now equivocal. “They’ve done some horrific things. They’ve been abusive to other humans.” Collectively, the men of the M.D.U. have murdered, attempted to murder, stabbed, kidnapped, extorted, swindled and brought fear to entire cities. There were victims of these crimes, and some of them are still living. They will have their own opinions about the need, or not, for mercy.
Within the M.D.U., staff members believe that the future of the correctional system lies in more M.D.U.s. “This is the future,” one unit nurse told me.
“Have people from other institutions visited, to learn about the model?” I asked.
“Yes,” Mr. Doherty said. Then he turned to his colleagues. “Didn’t we have people from Guantánamo?”
In the meantime, some researchers are proposing a more modest approach: building more “dementia-friendly prisons.” Such prisons might have cell doors painted in different colors to help confused inmates orient themselves — and handrails, nonslip floors and accessible showers. They might guarantee that prisoners with dementia get bottom bunks and a bit more time to drop to the floor during drills. They might have pictures above the sinks to remind prisoners how hand-washing works and “scheduled toileting” for people who are incontinent. They might permit a person to wear Velcro clothing if he can no longer manage buttons or clasps. They could give him longer to finish his dinner.
Dr. Ruze, the clinical director, is skeptical of all of it. “In this country, we incarcerate way too many people for way too long. We give people life sentences. And then they turn 90, they’re in diapers, they get demented. We have to ask ourselves, what are we accomplishing?”
Whatever we are currently accomplishing or mean to accomplish, it seems to require that America’s prisons undergo a strange and maybe absurd conversion: into something that more closely resembles a locked-down, fenced-off, barbed-wire-enclosed nursing home.
As I left the M.D.U., a man was moving slowly down the hallway in a wheelchair, his head wrapped in a thick bandage — because, I was told, he bangs his head on the concrete walls when he gets frustrated. In the common room, another man was helping the person beside him to open a plastic container holding his lunch, a hamburger. Another man sat to the side.
“Do you like it here?” I asked him.
“Yeah, it’s fine,” he said. “But I’d rather be in … oh, what’s it …?” Then he forgot where he wished he could go.
Katie Engelhart (@katieengelhart) is a contributing writer for The Times Magazine and the author of “The Inevitable: Dispatches on the Right to Die.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips. And here’s our email: letters@nytimes.com.
Follow The New York Times Opinion section on Facebook, Twitter (@NYTopinion) and Instagram.
This post was originally published on this site be sure to check out more of their content.