This story first appeared in Bolts, and is reprinted with permission.
Michael Broadway gasped for air inside his cell at Stateville Correctional Center, a sprawling complex of beige and gray about an hour and a half southwest of Chicago. It was a sweltering mid-June day, when the heat index outside topped 100. Inside the crumbling prison, it felt even hotter, with one person estimating temperatures up to 120.
Anthony Ehlers and another of Broadway’s friends in a cell next door heard him say he was having trouble breathing and called out to a guard, according to an affidavit written by Ehlers. Roughly 15 minutes later, a nurse arrived, but she didn’t want to climb the stairs to Broadway’s cell. “It’s too hot. I’m not going up there,” she said, per the affidavit. “Tell him to come down here.”
By the time she ambled up the stairs several minutes later, Broadway was unconscious. His history of severe asthma was well-documented, and prison medical staff had prescribed him medications for the condition. Yet the nurse instead twice administered the overdose reversal drug Narcan as she yelled at Broadway to open his eyes, according to medical records and an affidavit from someone in the cell next door. Two guards in the cell took turns giving him chest compressions while she looked on.
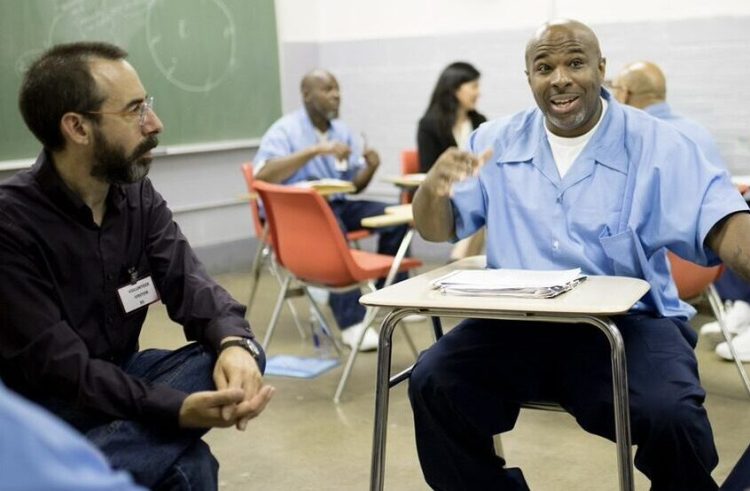
Michael Broadway, right, earned a bachelor’s degree from Northwestern University while incarcerated. He died in prison this summer. (Photo courtesy of Monika Wnuk)
The guards reached for the stretcher—but it didn’t have straps or handles. A man one cell over offered up his bedsheet and eventually helped two guards carry his friend’s limp body downstairs. By the time an ambulance arrived at the prison to take Broadway to the hospital, he wasn’t breathing and had no pulse. An autopsy later revealed he died of bronchial asthma, with heat stress listed among “significant contributing conditions.”
The medical care Broadway received at the end of his life is commonplace for the nearly 30,000 people incarcerated by the Illinois Department of Corrections (IDOC). Wexford Health Sources, the company the state has paid for prison health care services for decades, has long faced accusations of neglect and abuse, including enforcing a “one good eye” policy and providing such poor treatment to older people with dementia that court monitors compared it to elder abuse.
“Mike was far from the first, and unfortunately, he won’t be the last,” Ehlers wrote in a message to Bolts. “He died as a result of being less than in the eyes of the people who oversee us. … The staff in these prisons DO NOT see us as human beings.”
Terah Tolner, an attorney representing Broadway’s family, said his experience is “just one example of many of IDOC and Wexford’s pattern of delay and unpreparedness and inadequate medical treatment.” Illinois has been bound by a federal consent decree to improve the quality of treatment it provides incarcerated people since 2019, after a lawsuit alleging poor medical care triggered intervention by the courts.
Nonetheless, earlier this year, IDOC inked a 5-year, $4 billion contract with Wexford, raising fresh questions about the state’s commitment to improving quality of care for incarcerated people.
Sarah Grady, a civil rights lawyer who has represented a number of incarcerated people in lawsuits against IDOC and Wexford, is disappointed in state leaders like Governor JB Pritzker and Latoya Hughes, the governor’s pick to lead IDOC as interim director since March 2023 for awarding Wexford a new contract despite its tumultuous history.
“It was a really incredible opportunity for the governor and the state to really think about a model that does not embrace this privatization,” she told Bolts.
Pritzker, who has heralded progressive legal reform efforts like eliminating cash bail, did not respond to a request for comment. Naomi Puzzello, an IDOC spokesperson, declined to comment on Broadway’s death, citing an ongoing investigation. “The Department has not foreclosed any reasonable ways to provide healthcare services to the patients in its custody,” Puzello said in an emailed statement. “At present, the Department remains committed to continuing to provide medical services [to] the individuals in custody through its emergency contract with Wexford.”
Wexford also did not respond to multiple requests for comment.
State prison officials are constitutionally bound to provide a very basic level of care to the people they incarcerate. While there’s no express guarantee of health care in the U.S. Constitution, the Supreme Court ruled that prison staff cannot knowingly ignore incarcerated people’s severe illnesses. Writing in a 1976 opinion, Justice Thurgood Marshall established the standard when he held that “deliberate indifference to serious medical needs of prisoners” violates the Eighth Amendment’s prohibition on cruel and unusual punishment.
For much of the nation’s history, this care was provided directly by state prison or health authorities. But around the 1980s, as the number of people behind bars skyrocketed, privatization took root as state lawmakers began to outsource these and other functions. Today, roughly two dozen states use for-profit health care contractors.
The industry is now dominated by a handful of corporations, including Corizon Health, Wellpath, and Wexford. All three have long histories of lawsuits and problems with staffing and quality of care. Corizon paid Arizona officials $3 million in penalties over six years for chronic understaffing. In May, Massachusetts officials declined to renew their contract with Wellpath following complaints that the company routinely denied care and used restraints and solitary confinement on people experiencing mental health crises.
Wexford has a long and complicated history with Illinois dating back to the 1990s, when state officials first began privatizing prison medical care. In 2005, the company had secured a $547 million contract to provide health care services to most state prisons. The following year, Illinois prison officials opened an investigation into a deputy warden who was accused of also working as a paid lobbyist for Wexford in New Mexico. Then in 2008, a former IDOC director was sentenced to two years in prison for accepting $50,000 in bribes from lobbyists, including a Wexford lobbyist. (The company itself was not accused of wrongdoing in the case.)
By 2010, the prison watchdog group John Howard Association of Illinois was warning of serious deficiencies in the psychiatric care that Wexford provided inside the state’s main women’s prison. Around the same time, from his cell at Stateville prison, Don Lippert filed a typewritten complaint in federal court alleging that he was routinely denied treatment for his diabetes, causing him headaches and nerve damage.
Despite the mounting problems under Wexford, in 2011 the state nonetheless awarded the company a 10-year, $1.3 billion contract to provide virtually all medical care to people incarcerated in Illinois prisons.
That same year, Lippert teamed with civil rights lawyers to argue that “widespread and persistent mistreatment” of incarcerated people extended far beyond indifference among specific staff members and was “a consequence of overarching policies and procedures put in place and executed by both IDOC and Wexford.” Others eventually joined the lawsuit, and in 2017 U.S. District Judge Jorge Alonso granted class-action certification. A court-appointed medical expert, in a report accompanying Alonso’s opinion, concluded that the state “has been unable to meet minimal constitutional standards with regards to the adequacy of its health-care program for the population it serves.”
In January 2019, the parties settled the case. A five-year consent decree, included as part of the settlement, required IDOC and Wexford to overhaul their medical and dental services by increasing staffing, improving record-keeping, and implementing policies that better protect incarcerated people. An independent monitor was tasked with overseeing the reforms and regularly updating the court.
But as the lawsuit played out in court, medical care for incarcerated people remained dismal. In 2018, a medical expert told the court that of 33 deaths behind bars studied, 12 were preventable. Another seven, the report noted, might’ve been preventable, while five others could not be determined because the deaths weren’t adequately documented.

Michael Broadway during his graduation ceremony in November 2023. (Photo courtesy of Monika Wnuk)
Even now, bound by a consent decree, heinous treatment continues to plague Illinois prisoners. The independent monitor wrote in a 2020 report that one nurse continued to pass out medication despite being asked by a guard to check on a person who was drooling and unresponsive. In 2023, the monitor flagged the case of an 80-year-old man with dementia who drank bleach from a soda bottle that had been left in his room.
Wexford’s 2011 contract with Illinois expired in 2021. After decades of business with the state, millions of dollars in settlements, and a trail of horror stories, incarcerated people and advocates on the outside hoped perhaps a change was finally in order.
But the company continued to provide care in Illinois prisons while IDOC solicited bids for a new provider. It received just two: from Wexford and VitalCore Health Strategies. Prison officials scored the two proposals based on the providers’ capability and experience, technical ability and methodology, resources, references, commitment to diversity, and pricing, according to Puzello, the IDOC spokesperson. Once approved by an independent state purchasing officer, the IDOC commissioner, appointed by the governor, can officially enter into the contract.
In January, IDOC announced it was again choosing Wexford—this time to the tune of more than $4 billion over five years, with an option to renew for another five. Contract talks with Wexford remain ongoing. In June, IDOC extended an emergency contract with the health care provider through the end of the year while they finalize the terms of a new agreement.
In May, four months after IDOC announced that it was again choosing Wexford, Judge Alonso agreed to extend the consent decree and court monitoring of health care in Illinois prisons for another five years. In making his decision, Alonso noted that half of the staff positions Wexford is contracted to provide remained unfilled, medical staff continued to administer incorrect medications, and IDOC still had not developed a comprehensive set of health care policies nearly four years after a July 2020 deadline.
Alan Mills, executive director of Uptown People’s Law Center, is a perennial prison litigator and one of the lawyers fighting IDOC and Wexford in the Lippert case. He questioned the factors that IDOC considered in choosing Wexford over VitalCore, which bid lower for the contract. “Clearly, the quality of medical care being provided is not ranked high enough,” he said.
Mills told Bolts that for-profit companies like Wexford have “a built-in economic incentive to provide only the minimum level of care that gets your contract renewed.” Since contractors are paid a flat rate, rather than by the services provided, “every time they actually provide care, it comes off of their profits.”
A 2020 Reuters investigation found that, of 500 state jails surveyed between 2016 and 2018 across the U.S., those that contracted with one of the five largest private providers had higher death rates than those run by government agencies.
The issue is bigger than any one company, said Grady, the civil rights lawyer. Improving medical treatment for incarcerated people in Illinois requires a culture shift, where profit motives no longer drive decisions about care.
She called for greater oversight from state lawmakers, and she urged Prtizker and Hughes to think transformatively about a system that prioritizes quality of care over profit. (Pritzker’s office did not respond to a request for comment.)
“If you spend just a little bit of time looking at this system,” Grady continued, “there can be no doubt that it is not good for the state–including the taxpayers–and it’s certainly not good for the vulnerable people who are forced to suffer because Wexford is more interested in making a profit than caring for patients.
This post was originally published on this site be sure to check out more of their content.








